Background: Immune thrombocytopenia (ITP) is a bleeding disorder caused by autoantibodies against platelet glycoproteins (GPs). A key attempt to treat ITP is to eliminate the autoreactive B cells. Here, we proposed a new strategy for B cell-depletion therapy of ITP, chimeric autoantibody receptors T cells (CAAR-T), which could trap autoreactive B cells and perform specific killing. GPIbα is a significant autoantigen found in ITP patients and indicates a poor response to standard immunosuppressive treatments. We developed GPIbα-based CAARs in this study.
Aim: To precisely eliminate the autoreactive B cells to treat ITP.
Methods: We constructed various lengths of the native GPIbα ectodomain into the ligand-binding domain of a second-generation CAR structure and expressed the CAAR structure on the HEK293 cell surface to verify its conformational epitope. We immunized BALB/C mice with human platelet lysates to obtain anti-GPIbα hybridomas and performed a binding assay to confirm selected hybridoma antibodies' binding ability to GPIbα CAAR. We performed cytotoxicity assays to assess GPIbα CAAR-T-cell selective cytolysis against anti-GPIbα B cells in vitro and developed a xenograft model to assess the cytolytic efficiency and security of GPIbα CAAR-T cells in vivo. A plasma antibody binding assay was used to test GPIbα CAAR-T cells' ability in reaction with native GPIbα autoantibodies from ITP patients. We applied an enzyme-linked immunospot (ELISpot) assay to verify GPIbα CAAR-T cells' potential in eradicating autoreactive B cells of ITP patients.
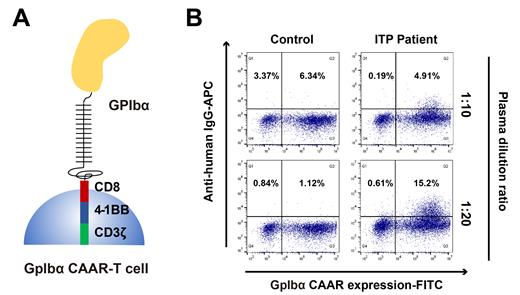
Results: We successfully expressed GPIbα CAAR structure on the cell surface and proved that the conformational epitope of GPIbα CAAR is consistent with that of the native human platelet GPIbα. The Schematic of GPIbα CAAR structure is presented in Figure 1A. By immunizing BALB/C mice with human platelet lysates, we obtained four anti-GPIbα hybridomas with different CAAR binding sites. Vitro cytotoxicity assays confirmed GPIbα CAAR-T-cell selective cytolysis of anti-GPIbα hybridoma cells. In a hybridoma xenograft model, we verified that the CAAR-T cells could persist and selectively lyse autoreactive B cells and subsequently reduce autoantibody titers without apparent off-target organ toxicity. Through the plasma antibody binding assay, we demonstrated that GPIbα CAAR could react with sera from ITP patients with anti-GPIbα antibodies (Figure 1B). ELISpot analysis showed that GPIbα CAAR-T cells successfully eliminated anti-GPIbα B cells from a patient with refractory ITP, and normal B cells were not destroyed compared to anti-CD19 CAR-T cells.
Conclusion: Our study provides a proof of concept for CAAR-T cell therapy to eradicate autoimmune B cells while sparing healthy B cells, which would compensate for the defects of traditional B cell depletion therapy in ITP. GPIbα CAAR-T therapy would be a promising treatment for refractory and relapsed ITP patients.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal